The link to the paper I’m writing about for my first Cystic Fibrosis (CF) Canada blog post can be found here1.
As I mentioned in my blog update, I’m now a blogger for CF Canada. My task at CF Canada is to write about the latest CF research being done by Canadians. I saw helping out at CF Canada as a great opportunity for me to connect more closely with the CF patient community and for me to practice making complex research approachable for the general public. It’s what I’m doing for you right now, but exclusively focusing on Canadians who specialize in CF research.
The first article I will share for CF Canada’s blog focuses on P. aeruginosa, the pathogen that I wrote about for my very first Microbe Musings blog post. Now if you recall, P. aeruginosa is the most dangerous pathogen that CF patients face. Preventing P. aeruginosa infection is a huge priority for CF clinicians, encouraging a lot of research for refining the treatment of airway infections. The use of antibiotics to treat infections spearheaded much of the infection control methods that improved life expectancy for CF patients. Chief among these antibiotics is tobramycin, which prevents P. aeruginosa and other bacteria from producing the proteins it needs to survive. As soon as P. aeruginosa is first detected, patients are administered inhalable tobramycin twice a day for 30 days to clear the pathogen before they can establish themselves.
The big problem arises when intense treatment with antibiotics like tobramycin fails to clear the P. aeruginosa infections. Once P. aeruginosa establishes itself in the CF airways, there is no way to eradicate them, even with intense antibiotic treatment. Many CF patients face this grim reality. Patients with permanent P. aeruginosa infection are more likely to experience accelerated lung damage and have an increased risk of death from respiratory failure2.
Two years ago, I attended a seminar led by Dr. Dao Nguyen at McMaster University. She was a visiting professor from McGill University who specialized in CF infections driven by P. aeruginosa. At the end of her talk, she barely had enough time to talk about how interactions between P. aeruginosa and the host immune system affect how well the patients fare against the deadly pathogen. Her work spurred my interest in studying P. aeruginosa infections for the latter half of my thesis and inspired me to showcase her work for my first CF Canada blog post! What’s even cooler is that her lab published a study earlier this year asking how intense tobramycin treatment could fail to clear P. aeruginosa infections when first encountered in the CF airways.
For their study, the Nguyen Lab sampled collected P. aeruginosa isolates from children who recently had their first P. aeruginosa infection. Every child in the study was exposed to inhaled tobramycin treatment twice a day for 28 days. After the treatment, the children were grouped based on whether tobramycin treatment eradicated PA from their lungs. The isolates from both groups then had a set of traits measured. These traits included their motility; their ability to generate slimy, mucoid colonies; and biofilm production, the ability to produce a tight community of bacteria attached to a surface.
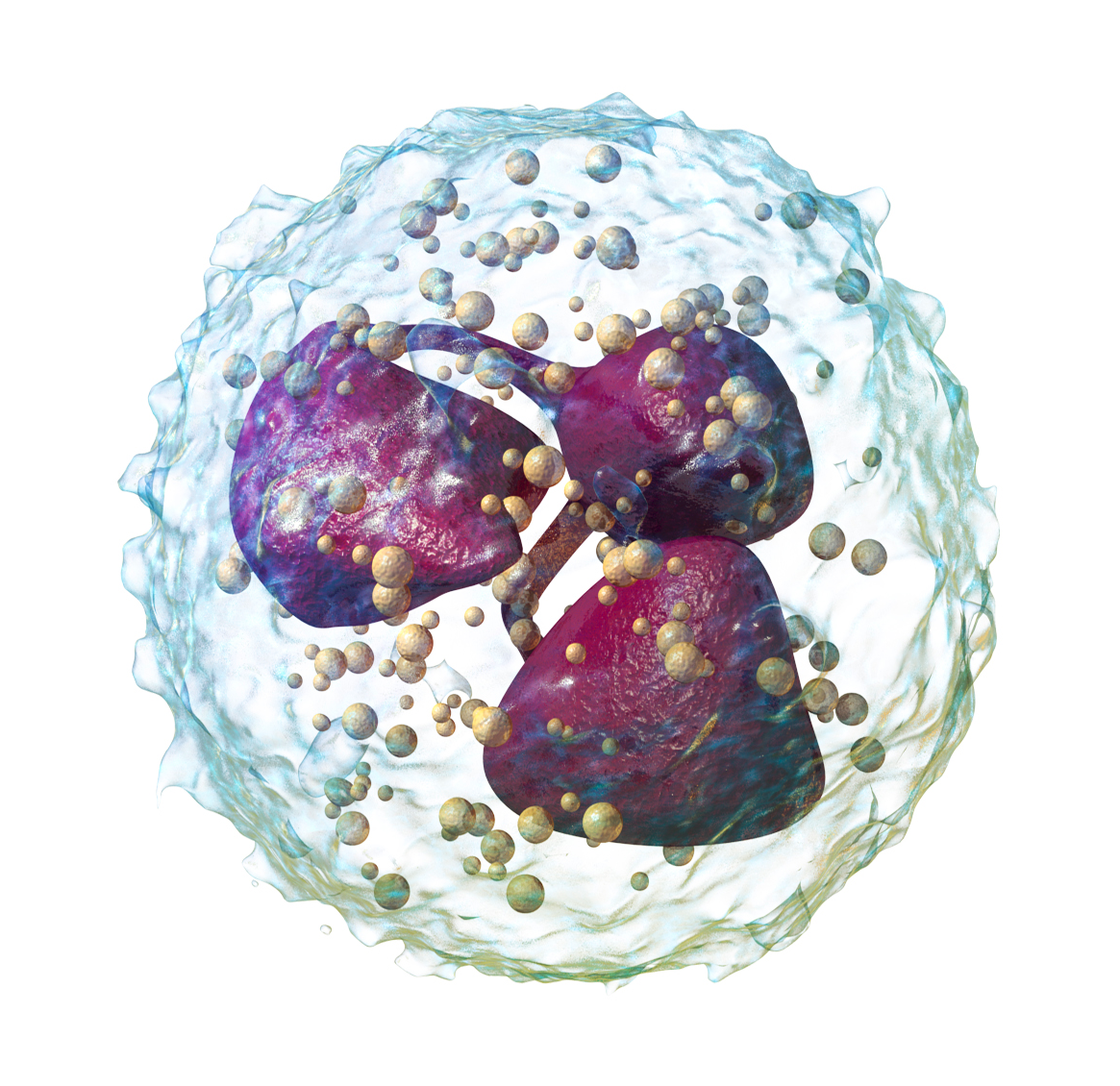
The key finding from the study lies in an important part of our immune system: the neutrophils. Neutrophils comprise 40-60% of the white blood cells in our bodies. When neutrophils encounter bacteria like PA, they perform phagocytosis, a process where the neutrophils swallow the bacteria whole for eating. This process ensures that the bacterial cells are unable to wreak havoc when they enter the host. The PA isolates that survived intense tobramycin treatment were resistant to phagocytosis by the neutrophils, whereas the eradicated isolates were more susceptible to phagocytosis. Interestingly enough, the resistance against phagocytosis was associated with reduced movement and the generation of slimy mucoid colonies. Both of these features are typical traits of bacterial aggregates clumped together in the mucus that protects bacterial cells from phagocytosis.
The fact that P. aeruginosa cells can survive intense antimicrobial treatment and host attacks so soon after first detection shows just how fast P. aeruginosa can adapt to the CF airways. What’s particularly concerning is that even when the P. aeruginosa infection is successfully treated, a different P. aeruginosa isolate can just come back and be more successful at colonizing the CF airways3. It thus becomes a game of cat and mouse to prevent P. aeruginosa from colonizing the CF airways for as long as possible to maximize patient life expectancy. Even with these difficulties, learning the traits that enable P. aeruginosa to survive antimicrobial treatment can help tailor future treatments to increase the chances of success for future CF patients.
To end this article, I want to share a cool Youtube video that shows the process of a neutrophil performing phagocytosis on a bacterial cell4. You can see the large neutrophil extending itself to swallow the cell and destroy the bacterium afterwards. In the CF airways, the mucus buildup and the characteristics of the bacteria infecting the airways prevent neutrophils from doing their job, contributing to chronic infections in the CF airways. The results of the study make me wonder what could be done to enhance the ability of neutrophils to kill the bacteria that try to colonize the CF airways. Is there a way to clear the mucus? Perhaps there is a way to make the bacteria more susceptible to the neutrophils. Regardless of the way, it’s clear that a way to help the immune system kill the bacteria in the CF airways is in order.
References
- Kwong, K.; Benedetti, A.; Yau, Y.; Waters, V.; Nguyen, D. Failed Eradication Therapy of New Onset Pseudomonas Aeruginosa Infections in Cystic Fibrosis Children Is Associated with Bacterial Resistance to Neutrophil Functions. The Journal of Infectious Diseases2021, No. jiab102. https://doi.org/10.1093/infdis/jiab102.
- Emerson, J.; Rosenfeld, M.; McNamara, S.; Ramsey, B.; Gibson, R. L. Pseudomonas aeruginosa and Other Predictors of Mortality and Morbidity in Young Children with Cystic Fibrosis. Pediatric Pulmonology2002. https://doi.org/10.1002/ppul.10127.
- Munck, A.; Bonacorsi, S.; Mariani‐Kurkdjian, P.; Lebourgeois, M.; Gérardin, M.; Brahimi, N.; Navarro, J.; Bingen, E. Genotypic Characterization of Pseudomonas Aeruginosa Strains Recovered from Patients with Cystic Fibrosis after Initial and Subsequent Colonization. Pediatric Pulmonology2001, 32 (4), 288–292. https://doi.org/10.1002/ppul.1121.
- https://www.youtube.com/watch?v=6hYirwZVQNI; credit to Garland Science for making the video
Thank you for reading this article! I wanted to give the CF community some love with this article since I spent so much time sharing SARS-Cov-2 related papers. The B.1.1.7 variant has become the predominant variant in Canada, its increased transmissibility on full show here. It’s put us Ontarians back at another stay at home order while everyone gets their vaccine shots and case counts get put under control.
Some bad news though. I tried getting an interview from Dr. Jawed, but she never got back to me with the questions I sent her. Despite this setback, I’m still going to go ahead with my current schedule of sharing other papers, including the kefir milk paper! I still have more CF papers on the way, and I plan to write more articles about diverse microbial topics in the future, so stay tuned!
Finally, the featured image are those of bacterial plate cultures, something I work with all the time! The plate on the bottom left looks far slimier than the others. That’s an example of the mucoid phenotype that I discuss in this blog post!

Well written. Lots of hopeful research questions to also consider 🙂
Another great article!